I’m beyond excited about this new research study. For anyone interested in the power of breath, it’s right up your alley. It illustrates a positive use of artificial intelligence (AI), a use eagerly anticipated by many: the capacity to diagnose hard-to-detect medical disorders. To my mind, this work represents a breakthrough in understanding the connections between breathing and mind, brain, and body well-being.
But first, a bit of background.
Why Neurological Disease Matters
Neurological disorders are the largest source of disability and the second leading cause of death worldwide.
The body of evidence that connects disorders of the gut, brain, movement, and well-being will continue to grow.
Parkinson’s disease (PD), once vanishingly rare, is the most rapidly growing of all these disorders. The number of people with PD increased from 2.5 million to 6.2 million between 1990 and 2015. The prevalence is projected to double again to over 12 million by the year 2040.
An important note here: Many people with neurodegenerative diseases like Parkinson’s and ataxias die not of the disease itself, but of issues that arise from it. Movement problems such as difficulty swallowing, for example, lead to aspiration pneumonia which, along with frequent hospitalizations, taxes an already weakened system.
The pandemic-level increase (the researchers’ term, not mine) in Parkinson’s can’t be attributed solely to an increasingly older population.
Other catalysts of Parkinson’s include increased use of toxic environmental chemicals and additives like pesticides, radon, GMOs, water toxins, and plastics. Trichloroethylene, a substance used in dry cleaning and other solvents, has a causal influence in Parkinson’s. Paraquat is another pesticide linked to Parkinson’s disease. (It’s worth noting that while 32 countries have banned its use, the United States continues to deploy it in for weed and grass control in growing quantities. (Just google it and you’ll find multiple sources that decry its toxicity.)
Part of my keen devotion to the study of Parkinson’s and other neurodegenerative diseases lies in their links with several of my passions: movement, dopamine, sleep, and the gut-brain axis. And these are areas that challenge many of us, and will do so further as we age.
One of my previous pieces explored new research highlighting intestinal permeability in Parkinson’s and a new test that can detect it years before its onset. This is an exciting new development, but one that is not widely or equally available.
At present, to diagnose Parkinson’s Disease is a decades-long process. The tests (lumbar punctures, MRIs, multiple blood tests) are invasive. And diagnosis is expensive. Consider the novel measurement of alpha-synuclein, a misfolded protein and indicator of gut-brain inflammation linked with Parkinson’s, which requires a lumbar puncture. Moreover, the progression of the disease has historically been difficult to track, and thus to treat effectively. This means that both diagnosis and understanding of progression isn’t accessible for most people with Parkinson’s.
And that leads me to this study from 2022 that I can’t believe hasn’t received more media attention, because of the novel diagnostic tool the researchers developed, and because of its potential applications to other illnesses.
The link between Parkinson’s and disordered breathing was noted more than two hundred years ago in the work of James Parkinson. Later work expanded on respiratory symptoms in PD, including weakness in respiratory muscles, disordered breathing in sleep (e.g. obstructive sleep apnea), and degeneration in brainstem areas that control breathing.
Like the intestinal permeability issues in the article I wrote and linked above, disordered breathing manifests years, even decades, before the motor symptoms of Parkinson’s appear.
This made me wonder deeply about the links between breathing and gut permeability.
I dug into the research just a little, and found a 2023 study. The researchers showed that disordered breathing during sleep can alter the fecal microbiome and impair the functioning of the gut epithelium (lining), which is shown to be compromised in Parkinson’s. This permeability leads in turn to higher levels of inflammatory molecules in the brain.
The causal relationship may also work in reverse. Researchers also think that intestinal permeability causes inflammation, which can affect breathing during sleep. I wonder if this is one reason why obstructive sleep apnea has grown in such alarming numbers in otherwise healthy people.
The Study
Enter the beautiful study in question. This was a collaborative effort conducted by a group of researchers from the Massachusetts Institute of Technology, Rutgers University, the University of Rochester Medical Center, the Mayo Clinic, the Division of Sleep Medicine and Movement Disorders at Massachusetts General Hospital, the Boston University College of Health and Rehabilitation, and Emerald Innovations in Cambridge, MA.
The researchers evaluated 7,671 people from several hospitals in the United States, as well as public sets of data.
They developed an Artificial Intelligence (AI) model that used nocturnal breathing signals to detect and track the progression of Parkinson’s disease. (I must say that they discussed this rather nonchalantly and without fanfare in their paper; to me as a layperson, however, it was eye-poppingly exciting.)
The AI system collects breathing signals from a belt worn on a person’s chest or abdomen for just one night of sleep. It detects breathing pattern data from radio waves that bounce off the person’s body while they slumber.
The AI-breathing belt system not only reliably diagnoses Parkinson’s, but can estimate PD severity and progression over time—which, as stated, has been confoundingly hard to do.
The system is low cost and ideal for home use. It can be used repeatedly over time. It circumvents the need for costly in-hospital and in-lab sleep studies, which many U.S. insurance companies don’t pay for.
Further Implications
Gaping with delight at this study, I wondered about the future of breathing patterns as a diagnostic tool for other neurodegenerative diseases like ataxias, ALS, and Alzheimer’s.
And then I saw it: tucked surreptitiously into a corner of the paper, the researchers modestly noted that their AI tool also happens to accurately diagnose Alzheimer’s disease, too.
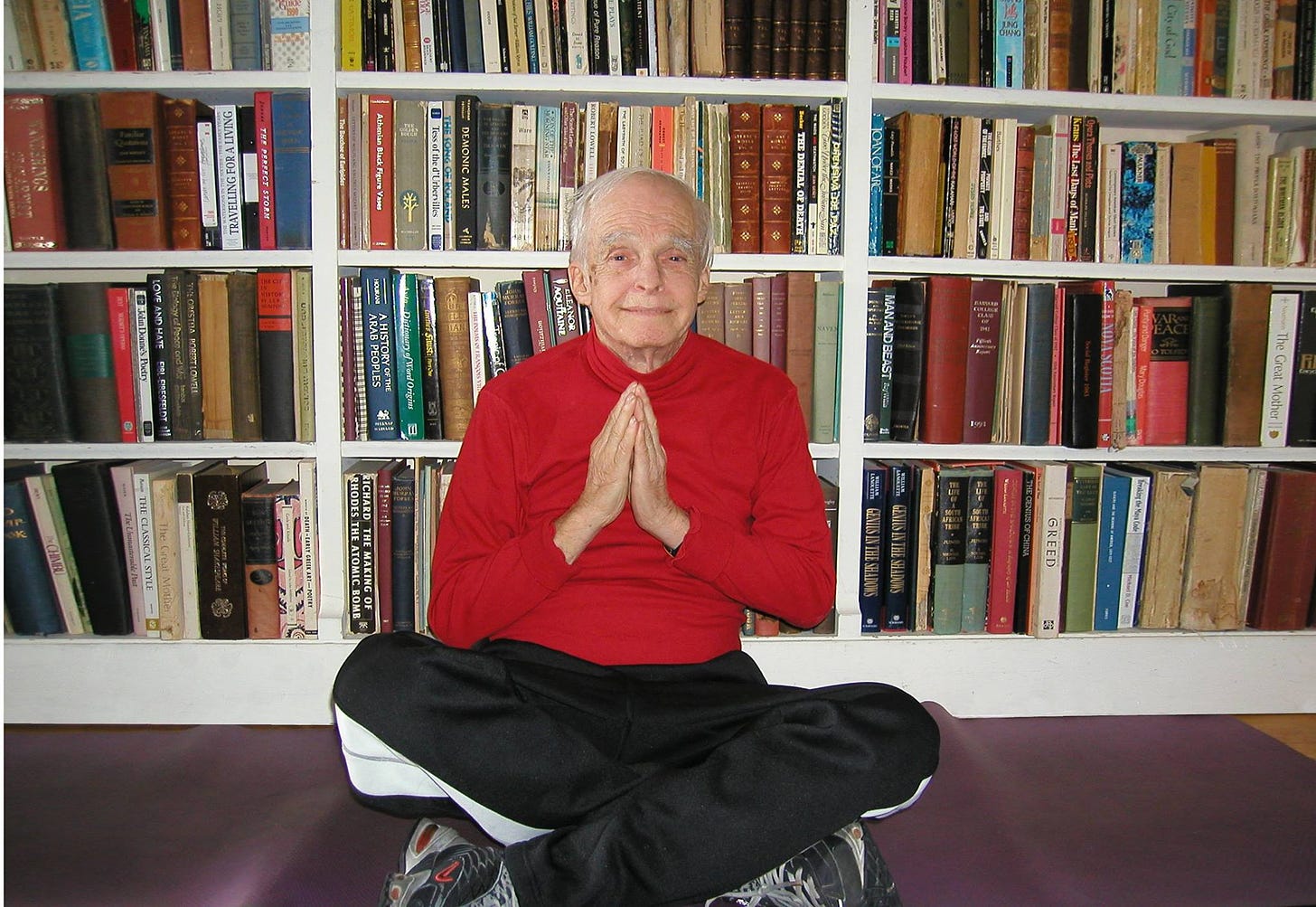
I’m reminded of my dad, who contended with Fragile X Tremor Ataxia, another neurodegenerative disease. I remember with clarity the startling improvement that five weeks of breath retraining, and then breath-centered yoga, levied on his movement, coordination, cognitive and emotional health, and social well-being.
I’m sure I’m not the only one to think it: If disordered breathing can cause intestinal permeability issues, motor dysfunction, and neurocognitive decline, what might breathing be able to offer as a therapeutic tool for the prevention and treatment of gut disorders and neurodegenerative diseases, particularly when caught early?
I’ll be keeping my eyes peeled for more.
Sources:
Neurological disorders are the largest source of disability worldwide: Dorsey ER, Sherer T, Okun MS, Bloem BR. The Emerging Evidence of the Parkinson Pandemic. J Parkinsons Dis. 2018;8(s1):S3-S8. doi: 10.3233/JPD-181474. PMID: 30584159; PMCID: PMC6311367.
And the second leading cause of death: GBD 2015 Neurological Disorders Collaborator Group (2017). Global, regional, and national burden of neurological disorders during 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. The Lancet. Neurology, 16(11), 877–897. https://doi.org/10.1016/S1474-4422(17)30299-5
Between 1990 to 2015 alone, the number of people with Parkinson’s: GBD 2016 Parkinson's Disease Collaborators. Global, regional, and national burden of Parkinson's disease, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2018 Nov;17(11):939-953. doi: 10.1016/S1474-4422(18)30295-3. Epub 2018 Oct 1. Erratum in: Lancet Neurol. 2021 Dec;20(12):e7. PMID: 30287051; PMCID: PMC6191528.
trichloroethylene, a substance used in dry cleaning and other solvents: Dorsey, E. R., Zafar, M., Lettenberger, S. E., Pawlik, M. E., Kinel, D., Frissen, M., Schneider, R. B., Kieburtz, K., Tanner, C. M., De Miranda, B. R., Goldman, S. M., & Bloem, B. R. (2023). Trichloroethylene: An Invisible Cause of Parkinson’s Disease? Journal of Parkinson’s Disease, 13(2), 203–218. https://doi.org/10.3233/JPD-225047
Paraquat is another pesticide linked to Parkinson’s disease: Spivey A. (2011). Rotenone and paraquat linked to Parkinson's disease: human exposure study supports years of animal studies. Environmental health perspectives, 119(6), A259. https://doi.org/10.1289/ehp.119-a259a
And when I dug just a little into the research, a 2023 study showed that: Li, Q., Xu, T., Shao, C., Gao, W., Wang, M., Dong, Y., Wang, X., Lu, F., Li, D., Tan, H., Jiang, Y., Xie, Q., Cai, F., Feng, L., & Li, T. (2023). Obstructive sleep apnea is related to alterations in fecal microbiome and impaired intestinal barrier function. Scientific reports, 13(1), 778. https://doi.org/10.1038/s41598-023-27784-0
They developed an Artificial Intelligence (AI) model that used nocturnal breathing signals: Yang Y, Yuan Y, Zhang G, Wang H, Chen YC, Liu Y, Tarolli CG, Crepeau D, Bukartyk J, Junna MR, Videnovic A, Ellis TD, Lipford MC, Dorsey R, Katabi D. Artificial intelligence-enabled detection and assessment of Parkinson's disease using nocturnal breathing signals. Nat Med. 2022 Oct;28(10):2207-2215. doi: 10.1038/s41591-022-01932-x. Epub 2022 Aug 22. PMID: 35995955; PMCID: PMC9556299.




Incredible! Thank you! Why isn't this information all over the front page of the New York Times?
"This permeability leads in turn to higher levels of inflammatory molecules in the brain. The causal relationship may also work in reverse. Researchers also think that intestinal permeability causes inflammation, which can affect breathing during sleep." Wow.